

This article is part of your HHCN+ membership
The home health industry has a high concentration of nurses who are closer to retirement age. Providers see the advantages and disadvantages of having an aging workforce.
In general, the registered age of the nursing workforce varies based on practice designation.
In home health and hospice, the number of nurses who are of retirement age is set to outnumber new RNs, according to data from the American Group Medical Association.
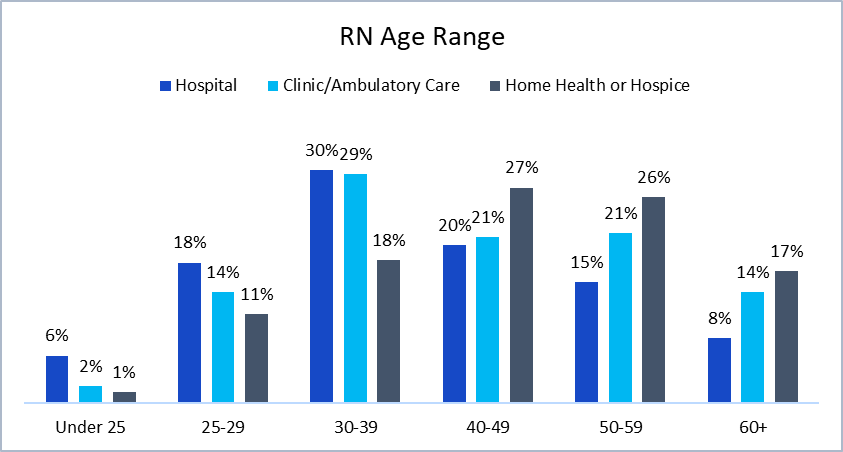
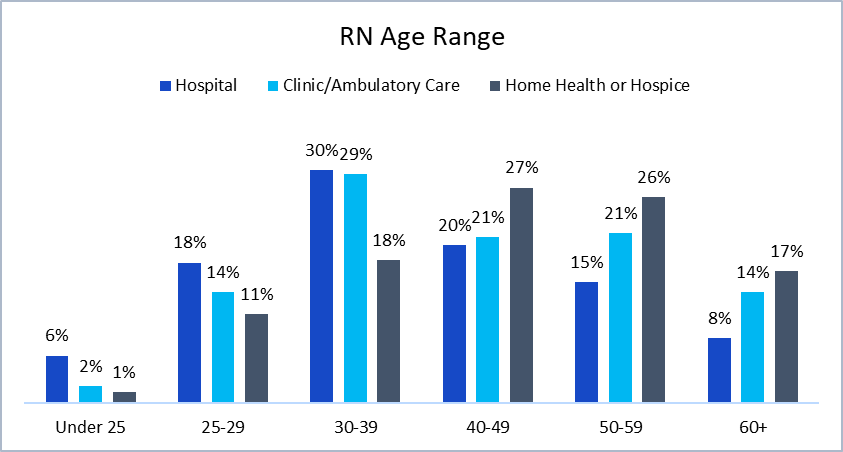
For context, the average retirement age is 63 for women and 65 for men, according to data from the US Census Bureau.
One of the reasons that nurses near or near retirement age make up a large portion of the home health industry is because newly graduated nurses are typically not being trained to provide home care while in school.
“You don’t have nursing schools that are doing home training, they’re really focused on facility-based settings,” Katy Barnett, director of home and hospice care operations and policy at LeadingAge, told Home Health Care News. “Sometimes you’re lucky to get someone with training in the long-term care facility space, but it’s very rare at home.”
On the other hand, Barnett noted that experienced nurses are often drawn to home health care.
“We’re really looking at nurses with years of experience in other settings coming into home health, for a lot of flexibility, but also knowing that they have that kind of clinical capacity to really serve patients themselves. she said. “They feel comfortable and confident serving that patient when they don’t have a clinical supervisor down the hall.”
The ability to feel safe providing care at home is especially important because it’s an environment that calls for autonomous decision-making, according to Mary Carr, vice president of regulatory affairs at the National Association for Hospice and Home Care (NAHC).
“You have to make a lot of decisions independently at home, you don’t have other nurses or clinical staff to lean on like you do in a hospital,” she told HHCN. “I just think it’s the preferred environment for someone who is an experienced nurse.”
Another benefit of having a workforce full of mostly experienced nurses is that they are better equipped to deal with burnout, according to Barnett.
“They’ve been through a lot and seen a lot,” she said. “They understand the workload they’re taking on, so the burnout rate is a little lower.”
At Masonicare—a nonprofit senior care provider based in Wallingford, Connecticut—15% of nurses are over age 60.
“In the last year and a half, when I looked at the numbers, we actually hired four patient-facing nurses between the ages of 60 and 63,” Laurie St. , told HHCN.
As a company, Masonicare operates the full continuum of care, including independent living, assisted living, skilled nursing facilities, memory care and continuing care retirement communities (CCRCs) on three main campuses. The company also offers home health, hospice and palliative care, plus inpatient behavioral health.
St. John has noticed that working with more experienced nurses has meant less turnover.
“Our highest turnover is in first-year nurses,” she said.
Although nurses nearing retirement age often bring a wealth of experience to their jobs, there are still downsides to an aging workforce.
“You really want people to experience the benefits of retirement, but that leads to problems in the overall nursing pipeline, and I think that’s one of the significant drawbacks,” Barnett said.
Plus, the departure of experienced nurses could mean an industry-wide brain drain of knowledge and vital history.
“Home health and home community services have really come of age in the last 20 and 30 years, so these nurses who are retiring … have been pioneers in this field,” Nicole Howell, told HHCN. director of workforce public policy at LeadingAge. “They’ve seen the really early stages now, the more exhausted system and the changing needs of both the individual receiving care and the families who are there to support them. As they move on to the next stage of their lives, we’re losing not only actual care knowledge, but really institutional knowledge of the sector and how far we’ve come.”
Masonicare has been able to avoid this brain drain, company-wide, as its nurses who are reaching retirement age often move into non-patient-facing roles. Many of these nurses move into mentoring roles that allow them to mentor other nurses in the company.
Additionally, many of these nurses who have moved away from visiting patients have played a major role in the company’s efforts to improve its orientation process.
“We rebuilt our orientation process and these nurses were critical in helping us,” said St. “We did focus groups with our nurses because we wanted to hear from them – what supports you best. As a result, we have added some resources to our quality and education team.”
#hidden #advantages #older #workforce #home #health #care
Image Source : homehealthcarenews.com


